Digitized X-Rays (CRMA)
CRMA stands for Computerized Radiographic Mensuration Analysis. Many times this process is referred to as “digitized x-rays.”
This is a test that Analyzes the angles and distances between bones in the spine using a Computer and X-rays, which are a certain type of Radiograph. The purpose of the test is to accurately assess damage to the spine.
Mensuration has been used by doctors for nearly 100 years to figure out when a patient’s spinal bones are misaligned. Mensuration compares a patient’s spine to a normal spine.
Why use CRMA?
CRMA is important to patients, doctors, and attorneys. For patients, it visually identifies the location of an injury. It also helps them understand common defenses to whiplash injuries are smokescreens invented by insurance companies. Finally for patients, it can explain the patterns of pain they experience as follows:
AMA Guides, p. 377 (5th ed. 2001)
AMA Guides, Fig 15-1, p. 377 (5th ed. 2001)
For doctors, CRMA assists with a “differential diagnosis,” which is the process doctors use to rule out other sources of pain. Insurance companies like to blame other sources as causes for pain, such as “somatoform disorder,” “secondary gain,” and other buzzwords that really mean someone is faking. CRMA objectively disproves faking. Since CRMA identifies the location and extent of injuries, it helps the doctor decide on a treatment plan targeted at the injured area. It is also helpful for tracking changes in a patient’s condition and for deciding when to make referrals to pain management specialists, neurologists, or surgeons. Many doctors take repeat x-rays every 3-5 years to monitor their patients’ conditions.
For attorneys, CRMA visually provides objective medical evidence of injury, which helps prove the patient’s injuries in court. In order to introduce scientific evidence in court, it must be reliable and scientifically sound. Because CRMA uses decades-old mensuration techniques approved by the American Medical Association, it is acceptable for this purpose.
The Medical Basis for CRMA
The mensuration method most commonly used today comes from the American Medical Association’s Guides to the Evaluation of Permanent Impairment (AMA Guides). It is the gold standard for impairment evaluation. For instance, the Arkansas Workers’ Compensation Commission requires use of the AMA Guides, and almost all other doctors recognize them as authoritative. The AMA Guides say the only objective way to assess permanent spinal injury is to look for “motion segment alteration,” which is “rare absent trauma,” as follows:
AMA Guides, p. 379 (5th ed. 2001)
In some cases, motion segment alteration can be easily seen with motion x-rays:
However, sometimes you need a method of analysis when injuries aren’t so obvious. That’s where the AMA Guides come in, and here’s what they say:
AMA Guides, p. 379 (5th ed. 2001)
This statement is important for two reasons. First, it means a doctor must take the right x-rays to determine whether motion segment alteration exists. Most of the time in the emergency room following a car wreck, ER doctors DO NOT take these x-rays. Why not? The ER doc knows specifically what he’s looking for — broken bones — so he orders specific x-rays for that purpose. The doctor does NOT order the x-rays required by the AMA Guides because it requires forward and rear bending, which can make fractures in the neck too small to see on normal x-rays far worse. So, these bending x-rays simply aren't taken until the patient has had some time to heal. So, the tests to see if motion segment integrity is lost is performed later, because someone else treats the condition in a non-emergency situation. Also, a loss of motion segment integrity can be difficult to diagnose in the ER because tissue swelling restricts the movement necessary to obtain the proper bending x-rays required. Finally, the patient needs sufficient time to heal so the true, permanent extent of the loss of motion segment integrity shows up.
The statement is important for another reason. It tells us that motion segment alteration CANNOT be diagnosed from a physical examination. So, without the proper x-rays, one just can’t say what the true extent of spinal injury is.
Once the x-rays are taken, the angles and distances between spinal bones are precisely measured and compared to a ‘normal’ spine. The American Medical Association determines what is normal:
AMA Guides, Errata p. 4 (Mar. 2002)
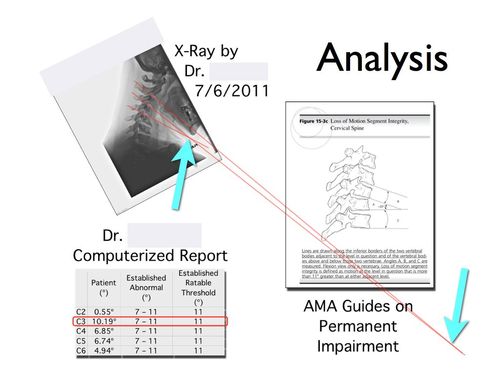
As shown here, in the neck any difference in angles more than 11º qualifies as a loss of motion segment integrity in the cervical spine. There are other figures available in the AMA Guides to measure different kinds of spinal abnormalities, as follows:
AMA Guides, Errata p. 4 (Mar. 2002)
AMA Guides, Errata p. 4 (Mar. 2002)
Current Methods in CRMA
Until the last 20 years or so, doctors performed mensuration by hand using x-rays, a light box, and a grease pencil. In the last 20 years, more doctors and clinics started using x-ray machines to take x-rays digitally, rather than with static films (just like digital cameras have replaced film cameras).
With the computing power available today, it also made sense for doctors to use computers to perform mensuration calculations. The result is a faster, more accurate, and repeatable mensuration report. One doctor we’ve spoken to says the hand-mensuration method took about 15-30 minutes, but the computerized version takes a trained technician only 30 seconds! That’s a huge time saver.
CRMA has been tested by researchers, who have confirmed it is more accurate and repeatable than hand methods. For this reason, CRMA is generally accepted in evidence-based medicine as a reliable method of assessing spine damage. Most research articles published on the spine today use computerized mensuration tools.
Case Study: Catching a Defense Doctor Cheating with CRMA
Below we show an example of mensuration performed by hand to show how errors can creep into the process. Can you tell what’s wrong with the image? Here’s a hint: it’s a small detail the doctor taking the x-ray overlooked.
Did you see the error? The patient’s chin isn’t touching her chest, which means the x-ray wasn’t taken at the full range of motion, which affects the accuracy of the result. The doctor who took the x-ray did so for an insurance company, and he had a reason to fudge the test. The doctor who performed the computerized report caught the error. And, the computerized report shows the angle is so abnormal a correct x-ray will likely show a loss of motion segment integrity.